Pelvic Congestion Syndrome - Common but Under Diagnosed Condition in Women
1. Introduction
a. This is also called pelvic varicosities, pelvic varices and ovarian reflux.
b. This is present in about 40% of women with chronic pelvic pain.
c. Chronic pelvic pain means pain in lower abdomen persisting for more than 6 months.
d. This is like the varicose veins that we see in the legs but the veins are the ones of the ovaries.
e. There is reflux (reversal of flow) in these veins that causes pooling of blood in the pelvis specially around the ovaries, vulva, vagina, inner thigh and sometimes around the buttocks and down the legs. This pooling causes the veins to dilate, bulge out and become knotty. As they dilate they increasingly pool more blood. Thus the term PELVIC VENOUS CONGESTION SYNDROME (PVCS). In the males this will lead to varicocele. As the testis reside outside the pelvis in males barring varicocele other symptoms usually do not manifest in the males.
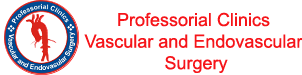
f. Normal Gonadal venous drainage VS refluxing drainage
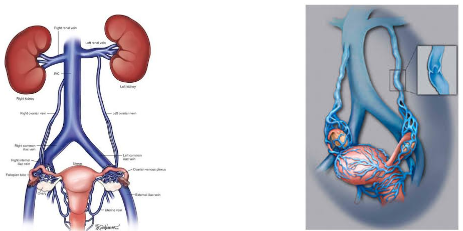
Figure 1
Direction of blood flow in the veins of the ovary should always be upwards as in the left sided diagram. When the direction of flow is reversed then the veins become bulgy, knotty and they pool blood leading to PVCS as in the right sided diagram.
2. Etiology
a. The valves that prevent backward flow are either absent or become incompetent.
b. In pregnancy there is increased blood flow and zone veins swell as a normal consequence of pregnancy. When the veins swell the size of the vein valves remain same as previous and reflux is expected. This should go away with childbirth. Some times it doesn't go away and you will have PVCS. This is the most common cause.
c. Sometimes there is an obstruction to upwards venous flow this can also lead to PVCS.
d. PVCS can also be consequent to polycystic ovarian disease.
3. Making the diagnosis
3. a) HOW THE PATIENT PRESENTS
I) Pelvic and lower abdominal pain.
II) Dragging sensation in the pelvis.
III) Worsening stress incontinence
IV) Pain more on standing.
V) Pain during sexual intercourse.
VI) Pain and fullness in the pelvis that may go right down to the legs
VII) Vulvar varicosities
3. b) HOW THE CLINICIAN WILL ARRIVE AT THE DIAGNOSIS
I) A patient presenting with above symptoms for more than 6 months is having CHRONIC PELVIC PAIN.
II) Complete history and physical exam with full exposure of the patient will reveal signs of PCVS as vulval, vaginal varicosities.
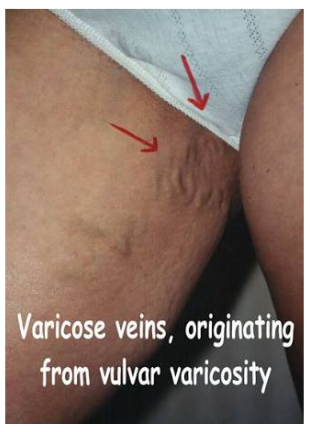
Figure 2
III) Imaging (Color Doppler ultrasound, CT angiogram, MR Venogram) these can make the diagnosis. Here I will stress that unless the ordering physician specifically requests a gonadal venous scan these are easily missed in routine imaging studies.
Classic CT scan of PVCS on the left and a dedicated text book MR venous imaging on the right.
IV) The gold standard of making/ruling out the diagnosis of is formal deep venogram. I usually will gain access to the deep venous system from your neck and reach the gonadal veins inject a contrast material that lights up the ovarian vein and confirm/rule out the diagnosis

The beauty of this procedure is that the reverse flow system can be closed right at the time we make the diagnosis with coils, chemicals or embolization particles.
Refluxing pelvic gonadal veins on the left and after closure by coils in the right as shown in
4. Management options
Usually patients do not want to undergo a procedures and will request for medical management. Medical management can reduce the pain and size of the varicosities in 75% cases. I MUST STRESS THAT THE ROOT CAUSE OF REFLUX IS NOT ADDRESSED HERE. The pain and size of veins can be reduces with medications like
a. Medroxyprogesterone acetate
b. Goserelin
These are not over the counter self-prescription drugs please be aware.
5. Risk Benefits of Endovascular procedure
This is the only procedure that addresses the root cause of the PVCS that is the reflux. It is successful in almost all the cases and has a success rate of 90% for 10 years. This means 90 of 100 PTS treated will be free of disease for 10 years but 10 will need repeat procedure in 10 years for recurrence.
No procedure is without risk. There are some risks associated with this procedure and they are as follows, they are very minimal and occur only in about 1 in 500 cases
a) Allergy to the contrast material.
b) Infection after the embolization procedure
c) Bleeding injury to target vessel
d) Non target embolization (distinctly rare) here vessel other that the intended one is embolized.
e) Radiation exposure
Conclusion:
1. PVCS IS A COMMON BUT UNDERDIAGNOSED CONDITION IN WOMEN WITH PELVIC PAIN OF MORE THAN 6 MONTHS.
2. Endovascular management is the only option that addresses the cause even though medicines will cause decrease in the symptoms in 75% cases.
3. This is a day care procedure and general Anesthesia is usually not needed.
Professor Dr Digvijay Sharma
Vascular Endovascular & Thoracic Surgeon
DMC 76008